Hospital ICUs are filling up. It’s even worse than it sounds.
As of mid-December, hospitals on average had just 22 percent of their intensive care unit (ICU) beds available across the country, and many were completely full. As the Covid-19 surge continues to intensify, lack of ICU beds can have dire consequences, including not being able to properly care for the sickest patients, potentially rationing lifesaving care.
But even these bed capacity numbers don’t tell the whole story.
Adding extra critical-care beds in other departments or buildings takes precious time, resources, and space. But adding trained staff is much more difficult, especially deep into a pandemic.
When trained staff are in short supply, it’s even harder for hospitals to best meet the needs of critical-care patients. These patients include people very sick with Covid-19, but also many who need to be in the ICU for other reasons, such as those who have had a heart attack or stroke, are recovering from major surgery, or are sick with the flu, among others.
Only about a dozen states had more than 30 percent ICU capacity left on December 15, and coronavirus case numbers have only accelerated since then. And the reality on the ground in many areas is much worse, as reporting by the New York Times has shown.
From the Times’s data, gathered from the US Department of Health and Human Services, of about 100 hospitals in the Los Angeles area, more than 65 reported ICU occupancy at 90 percent or higher. Cedars-Sinai Medical Center had an occupancy at 112 percent of its capacity.
In Dallas, the fourth-largest metropolitan area in the country, of the 47 hospitals with more than 20 Covid-19 patients, 80 percent of them had zero or just one ICU bed left. The most open beds any hospital had was five.
In the Minneapolis-St. Paul area, half of the hospitals with more than 20 Covid-19 patients were at more than 95 percent ICU bed capacity.
In Oklahoma, which has the third-highest per capita new case rate in the country, of the hospitals with more than 20 Covid-19 cases, the majority were at more than 90 percent ICU bed occupancy.
Nancy Nagle, a pulmonologist and critical-care physician at Integris health system in Oklahoma City, which reported full ICU occupancy in the most recent data to the HHS, says they have turned regular patient rooms into ICU rooms to try to handle the rush of severely ill people. Even so, she said, “occasionally Covid-19 patients must remain in the emergency department for several hours waiting for a bed to become available.”
And there is little sign of relief in many places around the country, with an average of more than 200,000 new Covid-19 cases reported daily since early December.
“Patients keep coming, and we have to take care of them regardless of our staffing levels,” Gisella Thomas, a respiratory therapist at Desert Regional Medical Center in Palm Springs, California, wrote to Vox in an email. “I worry that there is only so long staff can hold up before breaking, which ultimately, in itself, could limit capacity” further.
Covid-19 can be a long, unpredictable, complicated illness
The sickest Covid-19 patients can linger in the ICU for weeks — or longer. And although we have learned a lot since the spring about how to better treat severely ill Covid-19 patients, the disease itself is still challenging to address, and we don’t have a cure for it. Which means the 2 percent of people who get Covid-19 and end up needing critical care are often in ICUs until either they are able to recover — which often includes invasive intubation treatment — or die.
One of the reasons ICUs have been filling up is that once a patient with Covid-19 gets that sick, they are not likely to stabilize very quickly. A September study found that an average ICU stay for a Covid-19 patient was about a week — almost double the typical stay of 3.8 days for other ICU patients. Other anecdotal reports show that many patients can be in the ICU for weeks or even months. And pinning down this number is crucial for projecting how many beds might be available in the future if cases continue to climb.
As an October study pointed out, if an average length of stay in the ICU is 10 days, that means that every day there is only a 10 percent chance of a new bed opening up. So when admissions exceed that rate, ICUs are likely to get overwhelmed.
This is something those working with critically ill coronavirus patients have to contend with every day. “Covid-19 patients unfortunately stay in the ICU for a long time,” Nagle said. “The course of the disease is very slow, and this contributes to the shortage of available beds.”
And while Covid patients are there, meeting their needs can be extremely labor-intensive. “Covid-19 patients can be incredibly ill, with multiple machines to watch and adjust, multiple medications to give, and lab results to draw and results to watch,” Nagle said. And although we now have a better understanding of possible treatments for seriously ill patients, “patients still respond in varying ways, and their progress and possible outcome is always unpredictable.” This is another reason hospitals don’t always have a good projection for how many ICU beds they might have in the coming weeks or days.
Caring for Covid-19 patients also requires many more steps and precautions than when ICU staff work with other patients, further jamming units. All staff entering an ICU Covid-19 room must don full gowns and PPE each time, which is resource-intensive. “This also creates real difficulties if someone crashes because it slows down our response,” Thomas said. “The need to more thoroughly clean all equipment also creates delays and makes normal staffing levels inadequate for the pandemic.”
In the meantime, doctors, nurses, and other health care workers are struggling to provide the best care they can while being asked to handle more and more patients. “Critically ill patients are very complex,” said Orlando Garner, a pulmonary critical-care physician at Baylor College of Medicine. “There are a lot of moving parts at the same time that require the same amount of priority.” But, he said, “when you are stretched out beyond capacity, you can’t deliver the same quality care unless you create more skilled health care workers, and as we have found out, these are a scarce resource.”
Staff are even scarcer than ICU beds
Although hospitals can often somewhat expand the number of beds and amount of supplies, staff are in much shorter supply. “The most precious resource in any hospital are the human beings who are knowledgable and capable of caring for patients,” Sarah Delgado, an acute care nurse practitioner and clinical practice specialist with the American Association of Critical-Care Nurses, wrote to Vox in an email. “It is the limiting factor.” Without enough of these people to care for all of those who are very sick, “patient outcomes are likely to suffer,” she said.
And it is not just ICU physicians and nurses who are in short supply. “Critical care is more of a team sport,” Garner said. “This means physician-delivered care and interventions, but also careful medication selection dosage with pharmacists, skilled nursing care, respiratory therapists, midlevel providers, nutritionists, early mobilization with physical therapists.” To that list, Nagle also adds all of the other hospital staff needed to perform other essential tasks in ICUs, including bathing patients, changing linens, and other functions.
To accommodate surges of very ill Covid-19 patients, many hospitals have had to rework their staffing structure. At Christiana Hospital in Delaware, critical-care nurse Lauren Esposito and her colleagues typically work with critical cardiac patients. But this year, her unit has served as overflow for critical Covid-19 cases. “At first it was a little uneasy,” she wrote for the American Association of Critical-Care Nurses.
Their hospital implemented a tiered staffing strategy in which cardiac nurses would work under trained ICU nurses. “During the shift, if a patient was crashing, we were able to flex and have the ICU nurse go to that patient to provide care,” she wrote. They were also able to provide quick training to nursing staff, for example, on working with intubated patients. Still, the overflow duties were straining, and they weren’t made easier given the intensive isolation these patients are in to stop the spread of infection. “I remember the first time I walked into a patient’s room, it really hits you that you are the primary caregiver and no one else can come in.”
Also, staff now often have to attend to more patients at a time. In California, where last week an average of more than 44,600 people each day tested positive for the coronavirus, Gov. Gavin Newsom dropped the state’s nurse-to-patient ratio from 1:2 to 1:3 in an effort to meet the surging numbers of Covid-19 hospitalizations.
In Oklahoma, Nagle notes that although the ICU nurses she works with usually take care of one to two patients during a shift, “with the shortage of critical-care nurses, each nurse may have three, and under very extreme conditions, even four patients to care for.”
This increase in patients each nurse is seeing — especially in a complex illness like Covid-19 — is a major adjustment. “Nurses are at the patient’s side every hour of every day, administering lifesaving medications, collaborating with other health care team members, translating information to families, and providing end-of-life presence when those families cannot visit due to strict isolation requirements,” Delgado said. “This work cannot be done when the number of patients exceeds staffing capacity.”
And staff themselves often fall ill with the virus. According to a November report, as many as a quarter of Covid-19 infections in some states are among health care workers.
“It could have been me”
Garner, whose whole family got sick with Covid-19 earlier this year, including his 4-month-old daughter, says getting the illness himself gave him a new perspective on the patients now flooding into local Texas ICUs.
“It could have been me, my wife, or one of my kids on that ICU bed,” he said. “It’s easy to rationalize the amount of sick patients by thinking, ‘oh, well they weren’t distancing,’ or, ‘they weren’t wearing masks,’ but the fact is that nobody deserves to catch this virus and get sick from it, not even the people who doubt it. As the spike continues to grow, compassion is the only thing that can keep us from becoming jaded and burned out.”
The flip side of that is remembering compassion for the health care workers caring for these patients, especially as the holidays approach. Not only will many of these workers continue long shifts through the holidays, they will do so knowing that many people are disregarding public health warnings to avoid gatherings.
“We need the public to do its part,” Delgado said. “Stop nonessential travel, adhere strictly to mask-wearing and social distancing guidelines, and limit gatherings with those outside your household,” Delgado said.
Katherine Harmon Courage is a freelance science journalist and author of Cultured and and Octopus! Find her on Twitter at @KHCourage.
You May Also Like
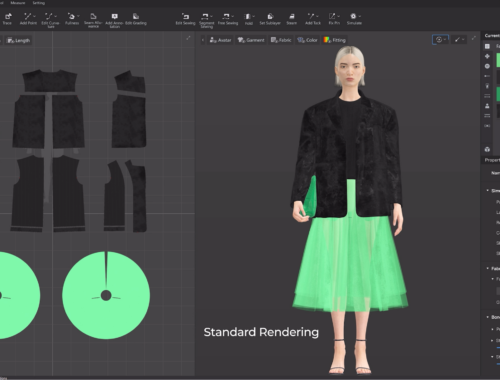
The Future of Fashion: How Artificial Intelligence is Revolutionizing the Industry
February 28, 2025
Generated Blog Post Title
February 28, 2025